The World Health Organization (WHO) last month acknowledged emerging evidence that coronavirus might be spread by tiny particles that can remain suspended in the air for hours.
By breathing, talking, coughing and sneezing, people produce aerosols that may, if the host is infected, contain pathogens. Most of the larger droplets emitted fall on surfaces within 1-2m from the source. A few larger droplets may, depending on environmental conditions, shrink by evaporation before they settle, to become an aerosol.
ASHRAE, among others, says small aerosols (less than 10 μm) can stay airborne and infectious for hours – even days – and, consequently, can travel longer distances and infect secondary hosts without contact with the primary host. The evidence has yet to be thoroughly evaluated, but – if confirmed – it will make management of indoor air quality even more critical for infection control and may lead to changes in government advice on measures to prevent the spread of Covid-19.
The design and operation of HVAC systems can have a major impact on infectious aerosol transport. Experts recommend flushing rooms with lots of outside air to dilute airborne concentrations of the virus. But increasing the volume of outside air might not be possible in all buildings (or weathers) and for all ventilation systems, which is why some experts are looking to ultraviolet light technologies as a means of limiting the transmission of coronavirus.
Ultraviolet (UV) light can inactivate a virus. There are three main types of UV radiation, classified according to their wavelength: UVA (400nm-315nm); UVB (315nm-280nm); and UVC (280nm-100nm). All three are present in sunlight; the shorter the wavelength the more harmful the UV radiation. UVA makes up the bulk of UV radiation reaching the Earth’s surface, and can penetrate deep into the skin. UVB can also reach the Earth’s surface and can damage DNA in our skin. UVC radiation is the most dangerous to humans, but is filtered out of sunlight by ozone in the atmosphere.
UVC is part of the ultraviolet spectrum that has the greatest germicidal effect. Its ability to kill bacteria was discovered more than a century ago. Since then, artificial sources of UVC – such as mercury lamps and, more recently, UVC LEDs – have been used to produce light with a wavelength of 254nm as a means of sterilising surfaces.
UVC light renders micro-organisms, such as bacteria and viruses, ineffective by destroying the genetic information in their DNA, so preventing them from reproducing and, effectively, inactivating the virus. When used in this way, UVC lighting is sometimes termed ultraviolet germicidal irradiation (UVGI).
UVC applications
A common use of UVC lamps is inside air conditioning units. Here, the lamps’ disinfection properties are employed to keep the cool, moist surfaces of cooling coils and drain pans free of mould, virus and bacteria. When the virus or microbe is on the surface, the lamps are able to deliver an effective dose. UVC lamps are also used to irradiate surfaces in labs and clinical spaces, but only when the rooms are unoccupied. This reduces the likelihood of virus transfer from objects and materials.
Signify, which manufactures UVC lighting, has been working with Boston University to validate the effectiveness of its UVC mercury vapour light source, with a wavelength of 254nm, to inactivate SARS-CoV-2, the virus that causes coronavirus disease 2019 (Covid-19). The researchers applied a dose of UV light with a radiant energy density of 5mJ/cm2; this resulted in a reduction of the SARS-CoV-2 virus of 99% in six seconds. Based on the data, it was determined that a dose of 22mJ/cm2 will result in a reduction of 99.9999% of surface bacteria in 25 seconds.
UVC is not the silver bullet, but it is good at getting to the virus in places where it is difficult to clean using conventional cleaning methods
A pre-paper by Beggs and Avital1 also found evidence suggesting that SARS-CoV-2, when suspended in air, is reasonably easy to inactivate using UV light at 254 nm. ‘Where you can shine a light, you will get UV disinfection on the surfaces where it falls; where there is shadow, there will be no disinfection,’ says Mike Simpson, global application lead at Signify, and CIBSE past-president.
When UVC is used for surface sterilisation, the number of fittings used is determined by the need to achieve a minimum irradiance level and by the need to eliminate shadows, says Simpson. ‘UVC is not the silver bullet, but it is good at getting to the virus in places where it is difficult to clean using conventional cleaning methods,’ he adds.
Safety has to be paramount when using UVC lamps; systems must be equipped with sensors and controls to ensure they only operate when people and animals are not present. ‘There should be no exposure to human skin or the eyes; if you are going to irradiate a room, you’ve got to do it in a way that ensures no-one is present when the UV lighting is on,’ Simpson says.
Signify has recently broadened its UVC offering of lighting fixtures to include devices to disinfect air, surfaces and objects. In North America, for example, a large retailer is piloting a UVC tunnel for disinfecting shopping trolleys. Other products include mobile, freestanding UVC luminaires and robot-mounted vertical lamps that can be wheeled into a hotel room or office.
While unshielded UVC lamps are used to disinfect surfaces in unoccupied rooms, upper-room air disinfection luminaires can be used in occupied rooms. These devices use shielded UVC lamps to create a germicidal UV zone at high level. ‘The technique for dealing with aerosol particles is to irradiate the air above the occupied zone,’ says Simpson. The upper-room units remain on all the time. Air disturbed by people moving around and by ventilation systems will eventually drift into the upper part of the room, where any aerosol droplets containing coronavirus will be zapped by the UVC, inactivating the virus.
If, however, air is moving too quickly, the virus will not be exposed to the UV light for long enough for it to suffer harm – which is why Simpson says ‘putting a UV light in ventilation ductwork is not effective’. A ‘belt and braces’ solution, he says, is to use upper-room air devices to disinfect the air continuously and combine this with unshielded lamps to disinfect surfaces at night, when the room is unoccupied.
Word of caution
Shaun Fitzgerald, co-author of CIBSE’s guidance on emerging from lockdown and a Royal Academy of Engineering visiting professor, acknowledges that UVC has been shown to be effective at inactivating viruses. However, he says the benefits of UVC can be marginal in well ventilated spaces: ‘If you have spaces that can be properly ventilated, then that is what I and other members of the CIBSE task group advise.’
Fitzgerald says, if you are pursuing a strategy of enhanced levels of ventilation, it is the law of diminishing returns for the use of UVC. ‘If you are doing an awesome job at removing the virus, then, to make a meaningful dent on the remaining virus with UVC – or any [air] cleaning technology – you’ve got to go at it really aggressively to get a lot of the room air through the system, which is just impractical,’ he adds.
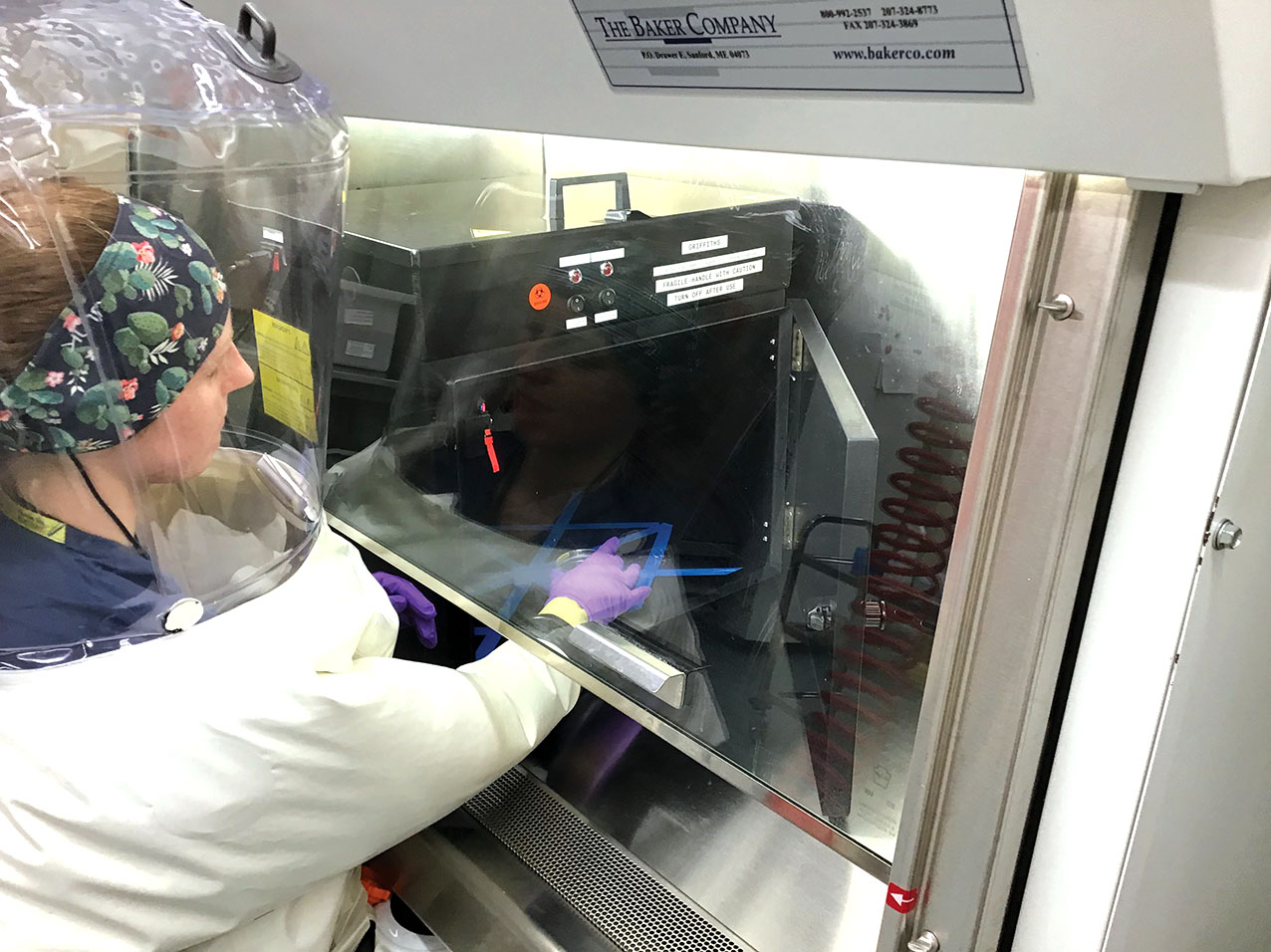
Research on UVC at the National Emerging Infectious Diseases Laboratories at Boston University
In spaces where it is difficult to flush with large amounts of fresh air, Fitzgerald says there are other technologies that may be worth turning to, and which may include UVC – but ‘it’s not what I’d turn to first’.
CIBSE coronavirus advice says that, in poorly ventilated spaces with high occupancy, ‘it may be appropriate to consider using air-cleaning and disinfection devices’. However, it cautions against an over-reliance on UVC: ‘There are currently uncertainties about a variety of factors affecting UV performance, including dosage, wavelength and exposure time.’ The advice also includes a warning that ‘any potential equipment will need to be properly tested, validated and quality assured, and demonstrated to provide the specific irradiation properties it is designed to and nothing else’.
Research from the US
Professor William Bahnfleth, of Pennsylvania State University, is chair of the ASHRAE Epidemic Task Force. He is in favour of UVC systems for germicidal irradiation as part of a multifaceted approach to limiting the transmission of coronavirus; this could include increasing outdoor airflow in a space, upgrading air filters and adding air disinfection equipment, such as UVC. ‘My hope is that the revised WHO position will result in more willingness to use all appropriate engineering controls to reduce airborne exposure, including UVGI,’ he says.
UVC might yet be a powerful weapon, but it is not a panacea… which is why face coverings, social distancing and hand washing are still necessary
According to Bahnfleth, germicidal UV technology has a long history in the US: ‘In the first half of the 20th century, upper-room systems were used to help control measles outbreaks in schools.’ The ASHRAE Handbook has two chapters on UVC fundamentals and applications, and the ASHRAE Journal has published articles on applications.3,4,5 In addition, he says studies of the effectiveness of upper-room systems have suggested that their ability to inactivate airborne pathogens in a space ‘may be equivalent to as much as 10 air changes per hour of outside air’.6,7
‘It is only my impression, but there seems to be a somewhat greater interest in, and willingness to use, air cleaners as adjuncts to ventilation and particulate filtration in the US,’ Bahnfleth says.
A study in the US by Columbia University is looking at the potential of UVC light, at a wavelength of 222nm, as a means of killing coronaviruses. UV light at this wavelength is known as far-ultraviolet C (far-UVC).8 According to the researchers, the advantage of using light at this wavelength is that it cannot damage human cells, so, potentially, would be safe for use in occupied public spaces to kill pathogens in the air before the occupants breathe them in.
To investigate how effective far-UVC light is at killing coronaviruses, a team at Columbia University Irving Medical Center aerosolised two common coronaviruses (the ones that cause coughs and colds), which it then flowed through air in front of a far-UVC lamp. The tests showed that continuous exposure to the far-UVC light in a room inactivated 90% of airborne viruses in about eight minutes, 95% in 11 minutes, 99% in about 16 minutes, and 99.9% in 25 minutes.
The team expect far-UVC to have the same impact on SARS-CoV-2. If successful, the research could lead to far-UVC lamps being retrofitted into existing light fixtures in buildings, aircraft and public transport, as part of a holistic approach to limiting coronavirus transmission.
Bahnfleth says the research is encouraging and, if far-UVC passes all safety tests for human exposure, it will open up new applications for germicidal ultraviolet. For example, safe germicidal UV could be used to treat occupied spaces, decontaminating both the air and exposed surfaces, displacing conventional upper-room technology. ‘It could open up a market of consumer disinfection products that would be safe to use and could be used for applications such as disinfecting elevator cars, toilet stalls, and other spaces for which it has been hard to identify good decontamination approaches using existing engineering controls,’ he says.
UVC might yet be a powerful weapon against an airborne virus, but it is not a panacea. UV does not prevent someone from being exposed to infectious aerosols emerging from an infected person close by, nor will it prevent people from being exposed to heavier droplets ejected when people nearby cough or sneeze – which is why face coverings, social distancing and good hand-washing hygiene are still necessary.
However, the benefit of UVC – and far-UVC in particular – is that, even if researchers develop a vaccine against the virus that causes Covid, UVC technology does not suddenly become redundant. Rather, it will be in place to help inactivate more familiar viruses, such as influenza and measles, helping making public spaces, offices and transport safer and healthier. More importantly, it will be ready for when the next virus pandemic occurs.
References:
- Beggs, C B, Avital, E J, Upper-room ultraviolet air disinfection might help to reduce Covid-19 transmission in buildings.
- ASHRAE position document.
- ASHRAE, Ultraviolet Lamp Systems, 2016 ASHRAE Handbook – HVAC systems and equipment
- ASHRAE, Ultraviolet air and surface treatment, 2019 ASHRAE Handbook – HVAC applications
- Martin, S, Dunn, C, Freihaut, J, Bahnfleth, W, Lau, J, Nedeljkovic-Davidovic, A, 2008, Ultraviolet germicidal irradiation: current best practices. ASHRAE Journal 50(8):28-36.
- NIOSH, Environmental control for tuberculosis: basic upper-room ultraviolet germicidal irradiation guidelines for healthcare settings.
- Article in Public Health Reports from 2003.
- Buonanno, M, Welch, D, Shuryak, I, et al, Far-UVC light (222 nm) efficiently and safely inactivates airborne human coronaviruses, Scientific Reports 10, 10285 (2020).


