Alternative-scenario analyses were carried out to find options for improving the baseline and optimising the design
When winter internal temperatures of more than 30°C and cold-water temperatures of up to 30°C were reported in some of its new buildings, Health Facilities Scotland (HFS) could not ignore the serious legionella risk this presented.
It commissioned Mabbett and Associates and IES to undertake a study of the issues, which were attracting additional costs because of remedial retrofit measures. They dug into the data and found that, although the designs and the design-stage modelling showed the buildings complied with regulations and statutory overheating checks, there was a performance gap between design predictions and actual building operation.
Susan Grant, principal architect at HFS, says that in targeting higher levels of Breeam at new NHS Scotland buildings they were creating highly sealed and well-insulated facilities to reduce heating bills. And although the NHS was finding other ways around thermal discomfort, including retrofitting air conditioning split units – says Grant – this was ‘not fixing the underlying problems’.
NCM has little to do with real life and everything to do with compliance. The reliance we placed on that was ill-founded
The study found that reliance on government-sourced national calculation method (NCM) data during modelling produced compliant – but unrealistic – designs. ‘NCM has very little to do with real life and everything to do with compliance. Once we started to understand that during the four years we have been working on this, we realised the reliance we placed on that was ill-founded,’ says Grant. More accurate and deeper modelling at design stage could have identified and mitigated problems, she adds.
HFS has now proposed recommendations that the NHS could adopt to improve the design and construction of future buildings.
Cold-water issues
The study found that the cold water came into the buildings at around 6-8°C, but travelled in ducts shared with the hot-water pipes once inside. Radiant panels, which are constantly on, also sit in roof areas. So by the time the water got into the tank – where it stayed stagnant – it was already above 20°C. Staff were forced to dump full storage tanks of water every morning to allow fresh water in. The water tanks were also found to be three or four times bigger than required. Real-world turnover of water is much lower than in design guides, which are primarily used for sizing peaks, not averages, says Grant.
Based on previous studies by Mabbett, the average water demand for Scottish hospitals is only 0.8 L.s-1, which is equivalent to five taps in use at one time. There are 55 cold-water taps in the 20-bedroom ward block looked at in the study because they were provided for clinical and patient use. Given the number of fittings in each ward block, water turnover is unlikely to be a reliable way to maintain cold-water temperatures below 25°C, let alone the target of 20°C, says Grant. Many health centres in city areas do not need tanks, she adds, while – in rural areas – they should be sized based on existing data for water use.
Modelling outcomes
For the study, HFS chose two facility types – a health centre and a hospital ward block – that were generic enough to be repeatable. The method involved building two baseline models and then performing a number of alternative-scenario analyses to find options for improving the baseline and optimising the design.
When starting projects, there’s a massive imperative to get it right first time, and a short period of time in which to design it, says Grant. ‘Modelling involves testing variables: what if we make the windows taller, or increase the floor-to-ceiling heights, or change the building services? All of these could give millions of permutations. We cannot replicate that in a real project, which has to be on site in a few months. So we took out the pressure of the deadline to test various options that are most likely to give us solutions,’ she says.
Using its Virtual Environment software, IES performed baseline simulations using NCM data and more representative (improved) data from the Room Data Sheet, supplied by Mabbett and Associates. A series of sensitivity analyses were done to evaluate different scenarios –such as modifying window openings, trickle ventilators and lighting energy – to demonstrate how these factors can reduce overheating.
The results when using the improved data revealed a more prevalent risk that could lead to more than 1,000 hours of predicted overheating per year, compared to no overheating when using the NCM data. David McEwan, consulting director at IES, says modelling enabled them to reduce overheating to 90 hours per year in the hospital ward, and eradicate it in the health centre building.
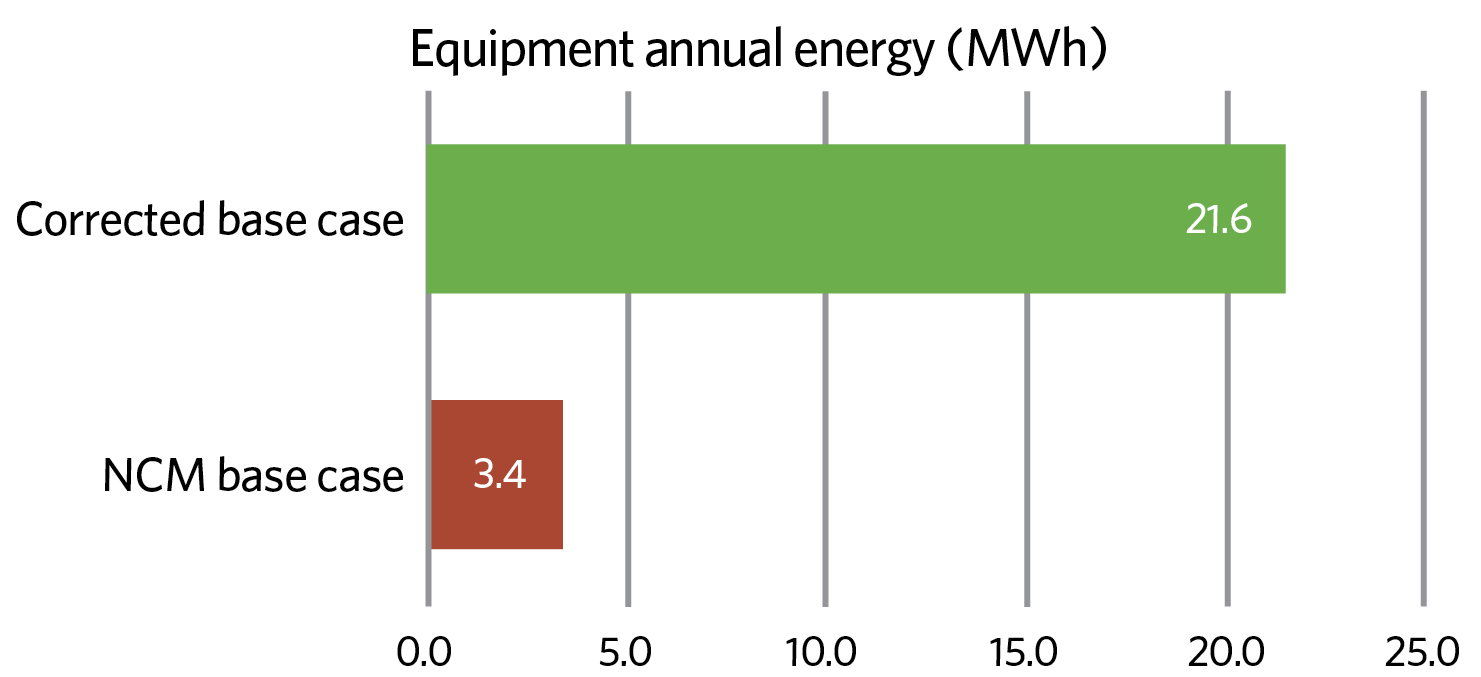
Figure 1: Equipment heat gains in hospital bedrooms using the corrected and NCM data
The greatest discrepancies between the data sets were over internal heat gains. For example, in hospital bedrooms the NCM assumes the energy consumed – and, therefore, the heat gain to the space – will be 3.4MWh per year for 20 bedrooms. The corrected base case, using real-world observations, is more than six times higher, however, at 21.6MWh (see Figure 1). In addition, no account is taken within the NCM data of distribution losses from hot pipework and other services in adjacent voids and rooms.
A lot of unintended background heat was detected when all service voids were modelled for the first time. As well as ventilating the voids, Grant says, HFS looked at insulating the pipework, which – after an initial drop in heat gains – didn’t make much difference. ‘We propose separating the hot service from the cold service by running them in different voids, or using point-of-use hot-water heaters,’ she adds.
The NCM model is built without ceiling voids, whereas the corrected baseline model includes a separation between the occupied room and the void. This means that in the more accurate model, there are lower lighting heat gains and higher gains from lighting controls in the voids, where the cold-water pipes are routed along with the hot-water services. ‘When we measured the heat generated by the LED controls in the service void above every room, we found that when air temperature outside was 9-10°C, ceiling voids were beyond 30°C,’ says Grant.
For the window design, daylight and thermal analysis helped to optimise window sizes and openings, but the solutions indicated an opening gap of more than 100mm, which is inappropriate in healthcare facilities, says Grant, so ‘future designs should focus on making sure trickle vents are sized properly to do their job all year round’. Simulations were also used to test for overheating using climate scenarios, including the CIBSE 2050 data set.
Climate-based daylight modelling should also be considered as the new standard because it allows you to choose the hours of analysis. This approach assesses when daylight is being used, so more accurate benchmarks can be defined when determining design scenarios.
Getting it right
HFS will use the report – published on its website – to generate new guidance for NHS Scotland. It has assembled a set of recommendations and design solutions that can be applied to new buildings, depending on the type of facility and its operating hours. ‘This can then be used to determine a target at the beginning of the design process. We would ask designers, through accurate modelling and sensitivity analyses, to prove the buildings are not only comfortable, but also thermally safe for water design, and the energy expectations of that in kWh per square metre,’ says Grant. Reviews will also be held at key stages of the design.
HFS also recommends using a soft landings approach, to feed real performance data back into the model to compare predicted with actual operation. ‘We hope to measure annual energy use for at least three years to see where further improvements can be made,’ Grant adds.
Although this approach to modelling can lead to better decisions being taken during design, NHS Scotland needs to ensure designers use accurate input data – based on real buildings – at each stage in the design process, says McEwan. ‘We need to get out of the vicious cycle of repeating the problems of the past by getting the right data at the right stage in the analysis. People can see the potential improvements we can make and, hopefully, they will start to do things differently. If designers do not build the right models, they’re not going to get improvements.’
HFS recommends a review of in-use energy within modern Scottish hospitals and health centres, to create recommended sets of load profiles for model inputs to be used by design teams. ‘This will provide more realistic data that designers in the UK can use to identify, and manage out, risks in their designs,’ says McEwan.