
The same system used to build stands at the FutureBuild conference in March were used to build the hospital bays
‘It was 6.15pm on Friday 20 March when the phone rang,’ recalls Stephen Cowlin, a director of building services consultancy The Richard Stephens Partnership (The RSP). ‘It was Ahmed Hassan, head of estates at Royal Free Hospital.’
He told The RSP to be at the ExCeL exhibition centre in London’s Docklands at 8am the following morning for a briefing with the NHS and the military.
On Saturday, Andrew Panniker, managing director of RFL Property Services explained that the NHS wanted to turn ExCeL into a 4,000-bed Covid-19 surge hospital. The army told Cowlin to treat it as a field hospital that has to be built quickly in response to an immediate need.
‘We normally start our design with the Health Technical Memoranda [HTM] and design down from this, with each derogation signed off,’ says Cowlin. ‘The army’s advice was to start with what it had and to work up from that to maximise what can be achieved in the timeframe available.’
The next day, The RSP heard that work was starting on site the following day and that the first 500 beds needed to be ready in seven days’ time.
The only facility big enough in which to house the 4,000 ICU beds needed to make up the predicted shortfall was the ExCeL centre
Cowlin says The RSP was asked to get involved because it had previously worked with the Royal Free London, which was initially in charge of getting NHS Nightingale London up and running. When Cowlin, a mechanical engineer, and fellow director Gerry Connor, an electrical engineer, turned up on site on Monday, they met James Hepburn, BDP principal, and his architect director colleague Paul Johnson, along with a small team of experienced healthcare architects and engineers.
BDP’s involvement followed a paper it had put together the week before, outlining the potential for convention centres to offer temporary facilities in which to treat coronavirus patients.
BDP’s architects had carried out space planning exercises, and concluded that the only facility big enough in London was the ExCeL centre.
‘On that first Monday, the brief was: we need 4,000 intensive care unit (ICU) beds all with oxygen, medical air and power,’ says Hepburn. NHS England also produced a guidance document for intubated patients [where a tube is fed through the mouth into the trachea], which set out what services each bed bay needed and the size of the bays.

The two 500m-long exhibition halls were converted into 80 wards each containing 42 beds
ExCeL comprises almost 90,000m2 of column-free space, divided into two 500m-long, 86m-wide halls located north and south of a 600m-long central boulevard. The deadline meant the Nightingale project had to use as much existing infrastructure as possible, which included the ventilation system.
When ExCeL is operating as an exhibition venue, giant 25m3·s-1 air handling units (AHUs) suspended from the roof provide heating, cooling and fresh air to the halls through high-level ducts fitted with high-velocity jet nozzles. Under normal operation, most of the air is recirculated in the AHUs to conserve energy, with air exhausted through passive vents in the 11m-high roof.
Cowlin says everything to do with the ventilation solution was developed in discussion with infection control specialists. His solution was to turn the halls’ existing AHUs into full fresh units, to supply a total of 300m3·s-1 fresh air to each hall.
Each AHU’s recirculation damper was physically blanked off and the roof exhaust vents were locked in a permanently open position. Some of the AHUs also supply the boulevard, so this solution ensures temperature and ventilation can be maintained in this space, too.
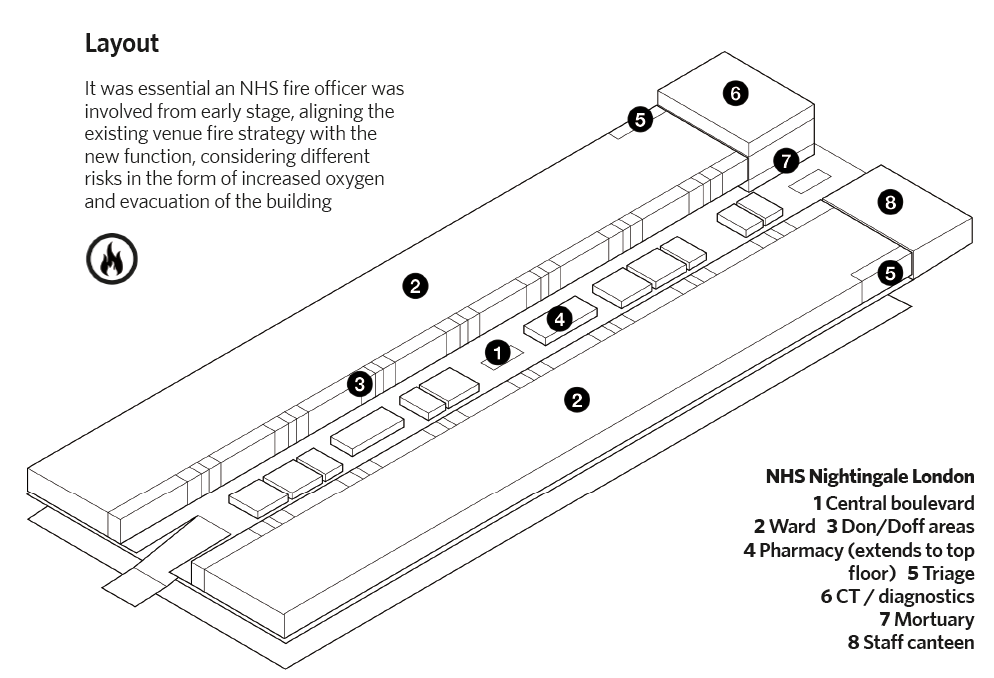
The layout taken from BDP's instruction manual for NHS Nightingale
The boulevard is classed as a ‘clean’ space, while the wards are classed as ‘dirty’. During an ExCeL exhibition, air would normally spill from the halls through 22 giant shuttered openings into the boulevard. The shuttered openings are now closed and sealed up to a height of 3m (to prevent virus-carrying droplets contaminating the space).
At full capacity, 16,000 staff will move from the clean corridor to the wards through sealed spaces termed Don and Doff rooms. Staff don their PPE in the Don rooms and remove it in the Doff rooms. ‘Using a simple arrangement of wall fans and a pressure relief damper, we’ve ensured the air always moves from the clean corridor to the wards,’ explains Cowlin.
Cowlin says because the AHUs are only supplying air to the halls, with no extract, he had to ensure the halls are not pressurised relative to the clean corridor so air is exhausted passively through the roof vents and it is ‘encouraged’ to leak out through openings in the external wall, where the dirty corridor is located along with the loading bays.
He says Infection Prevention Control (IPC) was not worried about HEPA filtering the exhaust because by the time the air has reached the external wall, it would not contain any infected droplets.
Cowlin says he was initially concerned that he might have to fit a false ceiling in the halls to achieve the air change rate recommended in the HTM for intensive care units.
However, because this facility was designed specifically for intubated Covid-19 patients, the air change rate was less critical. ‘The advice from IPC was that the virus is droplet-carried rather than airborne and although small droplets can be carried on the air, distances are relatively short so they were not concerned about the need for a high air change rate,’ he explains. Fresh air is mostly for staff. ‘We did calculations to demonstrate the oxygen enrichment is not needed,’ says Cowlin.
Electrical infrastructure
The event halls incorporate an underfloor network of ducts that feed a 5m x 3m grid of floor boxes, most containing data outlets and with the ability to connect to power and water; most boxes also contained a drain.
On day one, BDP’s architects set to work developing a bed layout. Working from the east end of the south hall, they positioned the beds in lines of 20 running from the boulevard to the external wall. The bedheads in one row back onto the bedheads in the adjacent row, and between them is a 1m-wide service corridor positioned above a row of existing floor boxes.
To build the bedheads, ExCeL put BDP in touch with GES, its exhibition stand builder, which uses a component-based system to construct stands. GES demonstrated the system’s capability by producing a series of six bays and bedheads. ‘The layout worked brilliantly, dictated by the floor box spacing and exhibition kit,’ says Hepburn.
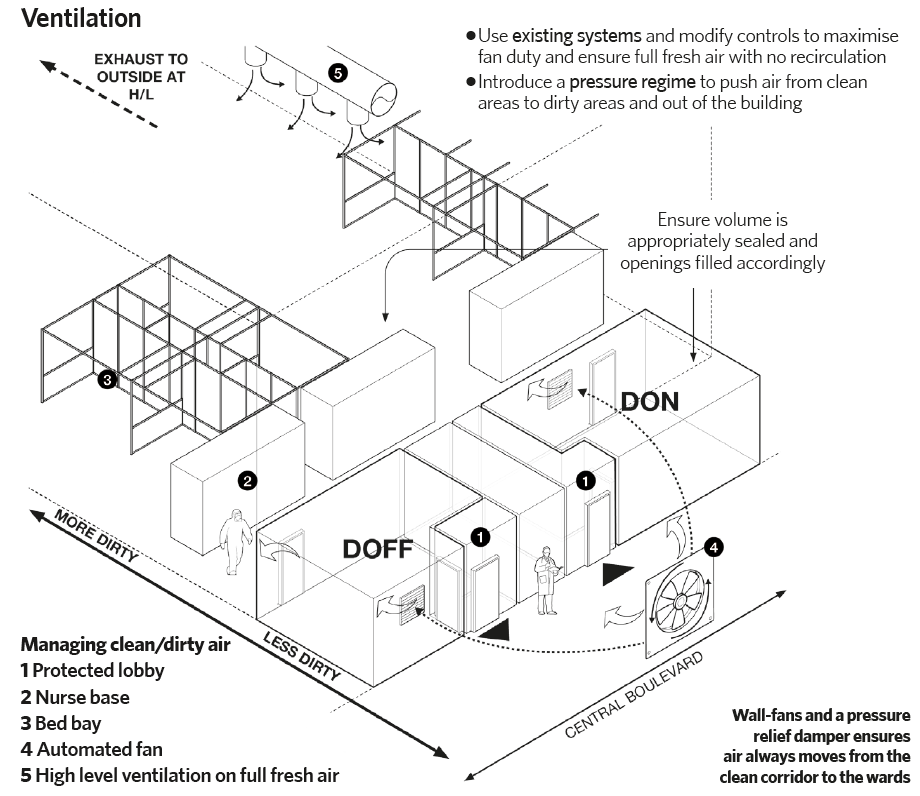
The ventilation design taken from BDP's instruction manual for NHS Nightingale
Meanwhile, the RSP’s Gerry Connor worked with ExCeL to establish how the electrical installation could be quickly repurposed. The north and south halls are each served by five service spines fed by a transformer supplying two 800A and one 400A busbars. The busbars run north-south beneath the hall floor linking the floor boxes via trenches running east to west.
During an exhibition, a tap-off box from the respective busbar enables power to be delivered to the stands using modular wiring terminated with commando sockets; the wiring connects through the floor boxes to a fused switch and then to a floor-mounted distribution board fitted with commando-socket outlets.
Connor decided to use the same system. He located the fused switches and distribution boards in the service corridor between bedheads. Sections of bedhead trunking were assembled on site by the electrical contractor using standard antibacterial dado trunking fitted with outlets for the medical gases and eight double-electrical sockets, nurse-call and a light switch for the bed light.
To enhance resilience, the bedhead was configured so that four of the electrical sockets are fed from one circuit, four from another. ‘We reused all of the exhibition kit for speed and flexibility,’ Connor says.
The bedheads were estimated to have a 7A load, which will be a significant electrical demand if all 4,000 beds are in use. But, because it was unclear what equipment was to be connected to bedheads it was decided that significant additional electrical loads come with their own power supply, such as mortuary fridges and CT scanners.
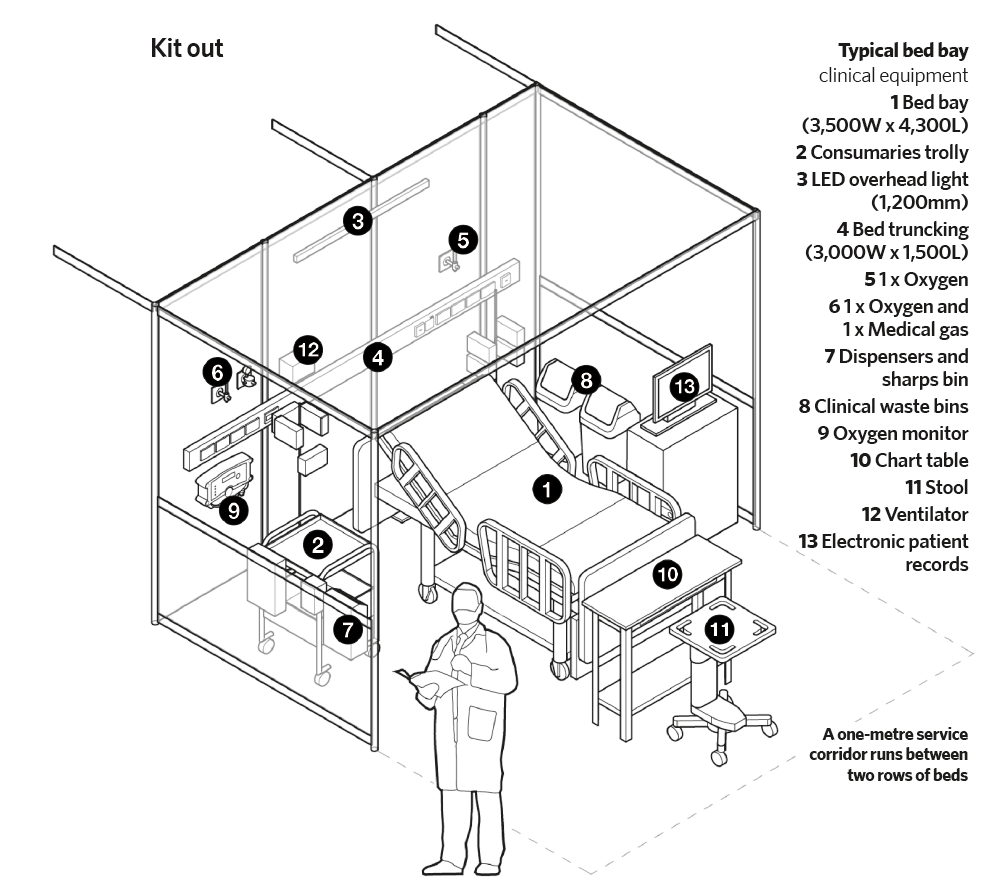
The kit out
Connor also had to enhance the electrical system’s resilience. There was an existing life-safety system at ExCeL, but only supplying escape lighting and security. Fortunately, there were two high voltage (HV) supplies. Switching from one to the other takes time because the HV ring needed to be de-energised and then re-energised, so additional resilience had to be added.
‘We had to put in a 600kW battery UPS and a 1600kVA generator to support what we called the essential busbar on each of the risers,’ says Connor. In total, 7.2MW of UPS and 19.2MW of generator provision will be provided to supply the bedheads. The UPS is sized to provide back-up for 30 minutes.
While this was going on a team from D&L Medical, led by Les Hood, was designing the medical gas system to supply the 4,000 beds (see panel ‘Medical gas’).
‘There was massive pressure to finalise the services design because all the services all had to be up and out of the floor boxes before they could lay the vinyl floor,’ explains Hepburn. BDP put together a series of ‘dot drawings’ to show: the floor boxes where the ExCeL team had to pull in a water supply and make a drainage connection; which boxes had a UPS-backed electrical connection, oxygen and medical air; and which boxes had a general electrical supply (not UPS-backed).
BDP instruction manual for NHS Nightingale
Hepburn says once installation work started it was ‘like an unstoppable juggernaut marching across the floors’. To keep it moving everyone was working 16-hour days.
Hoare Lea was brought on board to witness the designs independently and to take charge of commissioning the installation. It was responsible for the derogation schedule, which lists the reasons why a particular system has not been installed in line with the HTM.
Each derogation is signed off by the authorising engineer for every discipline and by the infection control expert.
NHS Nightingale London opened on 3 April and the first patients to leave were discharged just over two weeks later. After the first few patients were admitted, Cowlin says the temperature in the hall was reduced. Similarly the air change rate has been reduced so that it is just under two per hour.
Medical gas
D&L Medical developed a solution based on installing a new 108mm diameter oxygen main and a 54mm diameter 4bar medical air main at high level in the car park beneath the halls. Connections from the main feed up through the floor boxes. ‘Because we were trying to get this facility open in a week we needed more than 2,500m of 108mm diameter braised-jointed, degreased copper pipe installed along with 5,000m of flexible pipework to make the final bedhead connections,’ says Hepburn.
Oxygen is supplied from three new vacuum-insulated evaporator vessels that were being installed adjacent to the venue. The medical air system was to connect to four new triplex compressors.
